"white plague": an ancient infectious disease has never gone far.

Chest tightness, cough and phlegm, Wang Xiu thought she had a cold.
After a period of time, the symptoms did not disappear. Wang Xiu still felt very uncomfortable, so she went to the hospital for examination. After seeing Wang Xiu’s lung CT, the doctor told her that her lung infection was very serious and she had to be hospitalized.
Wang Xiu was hospitalized on the same day, and the nurse sent three sputum boxes, which not only collected her sputum at that time, but also asked her to collect the sputum that got up at night and in the morning respectively. Two days later, the sputum test showed that Mycobacterium tuberculosis was positive, and the doctor diagnosed that Wang Xiu was infected with tuberculosis. Because the hospital at that time did not have the conditions to treat tuberculosis patients, Wang Xiu was transferred to a specialized hospital. Worried about the possibility of misdiagnosis, Wang Xiu did a series of related tests, including sputum examination, blood drawing and filming, and was finally diagnosed as secondary pulmonary tuberculosis and bronchial tuberculosis.
"I thought it was just a lung infection. I might stay in the hospital for a few days, get some anti-inflammatory needles and use some antibiotics. I never thought I would get tuberculosis." Wang Xiu didn’t know how she was infected. After the diagnosis, she immediately reported sick leave to the unit leader and started the road of tuberculosis treatment.
What do we need to know about tuberculosis?
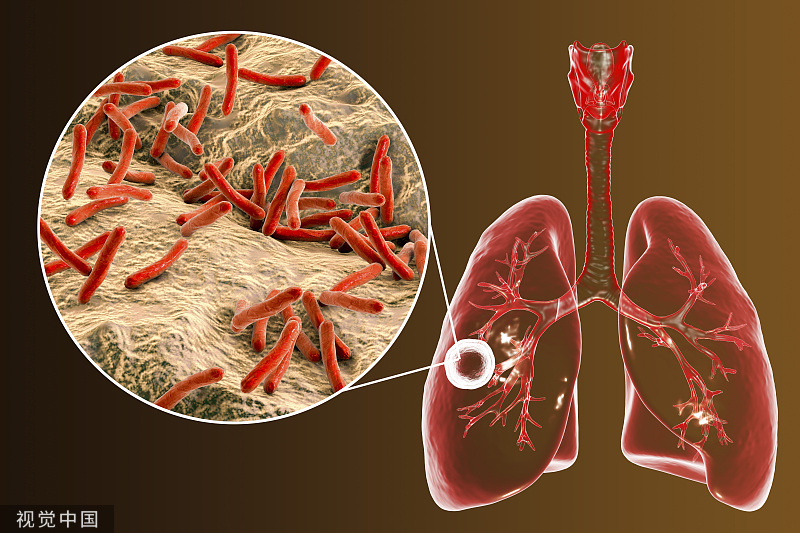
Tuberculosis, also known as "white plague" and "consumption disease", is one of the oldest infectious diseases in the world. It was once widely spread all over the world and claimed hundreds of millions of lives. However, a long time has passed, but tuberculosis has not gone far, and human beings are still plagued by tuberculosis.
According to the Global Tuberculosis Report 2022 released by the World Health Organization, it is estimated that 10.6 million people will suffer from tuberculosis in 2021, and a total of 1.6 million people will die of tuberculosis, which means that about three people will die of tuberculosis every minute.
China is one of the top ten countries with high burden of tuberculosis in the world, and the number of cases accounts for about 7.4% of the world. According to official statistics, from 2010 to 2021, there were about 10 million reported cases of tuberculosis in China, with about 30,000 deaths. In recent years, the number of reported cases and deaths of tuberculosis in China has shown an overall downward trend, but the scale of incidence is still large. The World Health Organization estimates that there will be about 780,000 cases in China in 2021.
Who are these patients? According to the analysis of the reported incidence of tuberculosis in China from 2015 to 2019, the majority of tuberculosis patients in China are men, and most of them are aged from 15 to mdash; Between the ages of 59, farmers are the group with the highest reported incidence of tuberculosis. The researchers pointed out that farmers have low awareness of tuberculosis prevention and control, poor economic conditions, and face many difficulties after being infected with tuberculosis.
"I have never known about this disease before, and I have never even heard of the name. At that time, I felt why I got this disease. I was scared and scared. " Before the diagnosis, Wang Xiu knew nothing about tuberculosis.
Tuberculosis is a chronic infectious disease caused by mycobacterium tuberculosis infection. Mycobacterium tuberculosis can invade many organs of human body, among which tuberculosis is the main one, accounting for more than 85% of all tuberculosis, and it is mainly transmitted by aerosol (droplets). The core information of tuberculosis prevention and control clearly points out that tuberculosis is a chronic respiratory infectious disease that seriously endangers people’s health. If cough or expectoration occurs, it will be ≥ 2 weeks, or with bloodshot sputum, you should suspect that you have tuberculosis. After you suspect it, you should go to the county (district) level tuberculosis prevention and treatment institution for examination and treatment. You can enjoy the national free policy for examination and treatment of tuberculosis in the county (district) level tuberculosis prevention and treatment institution, and as long as you insist on formal treatment, most tuberculosis patients can be cured.
Tuberculosis is very cunning. After entering the human body, tuberculosis does not attack immediately, but enters a latent state. Huan Shitong, a senior project officer of the Health Innovation and Cooperation Department of the Gates Foundation, once mentioned that TB will first test the immune resistance of the carrier. If you meet a person with strong immunity, then TB will enter a dormant state; However, once the host’s immunity is reduced, such as old age and illness, tuberculosis will immediately start "doing things" and reproduce and cause disease.
It is estimated that one out of every four people in the global population carries tuberculosis bacteria, of which 5%— 10% people may become tuberculosis patients in their lifetime. There are about 360 million people with latent tuberculosis infection in China, and one tenth of them may get sick. This figure is very alarming.
Risk factors leading to latent infection include immunocompromised patients (including HIV infection and iatrogenic immunosuppressant users), diabetics and the elderly. In 2015, the World Health Organization officially launched the guidelines for the management of latent infections, advocating the active detection and preventive treatment of latent infections in high-risk groups, and reducing the incidence rate through preventive medication. According to data estimation, preventive treatment of latent infection population can reach 60%— 90% protective effect, further reducing the incidence. Experts suggest that China’s tuberculosis prevention and control strategy has always focused on early diagnosis, early treatment and standardized treatment of patients, and has not yet formed a systematic intervention strategy for latent infected people. As a country with high burden of tuberculosis, it is worth discussing how to effectively carry out the intervention of latent infection to realize the rapid decline of tuberculosis incidence.
The treatment of tuberculosis is mainly drug treatment, which needs to follow the principles of early stage, combination, moderate amount, regularity and whole course. Drugs for tuberculosis can be divided into first-line drugs and second-line drugs, among which the first-line drugs have good curative effect and low toxicity, and can effectively treat most tuberculosis patients. Second-line drugs are either ineffective or toxic, and are used for patients who are resistant or intolerant to first-line anti-tuberculosis drugs. In China, ordinary tuberculosis patients can receive free drugs, including plate combination drugs and fixed-dose compound preparations. However, the current research and development of drugs for treating tuberculosis is extremely slow, and it was not until 2016 that the first approved new anti-tuberculosis drug appeared in more than 40 years.
What difficulties do tuberculosis patients face?
"The disease itself is not terrible, but the treatment time is too long, causing too much anxiety and psychological pressure." After the diagnosis, Wang Xiu faced both physical and psychological torture. Ordinary tuberculosis patients usually need at least six months of treatment to recover. During this period, Wang Xiu often feels loss of appetite, chest tightness, fatigue, dizziness and memory loss.
Despite these physical illnesses, Wang Xiu knows that tuberculosis can be cured, and more pressure comes from fear of discrimination. After the infection, Wang Xiu was afraid that her friends around her would panic, thus alienating her and staying away from her. But in fact, after the sputum test results of tuberculosis patients turn negative, they are not contagious and can contact others normally.
For drug-resistant tuberculosis patients, the situation is much more complicated. "I haven’t adapted to the side effects of these drugs yet." Ma Yi is a student suffering from multidrug-resistant tuberculosis. The disease brought him not only forced suspension of his studies, heavy family financial burden, but also serious drug side effects.
Ma Yi said that he didn’t know when he was infected with drug-resistant bacteria. Before that, he knew nothing about tuberculosis, let alone multidrug-resistant tuberculosis. Multidrug-resistant tuberculosis means that patients have developed resistance to common anti-tuberculosis drugs such as isoniazid and rifampicin. If the treatment is improper, the treatment scheme is not suitable, the patient stops taking drugs or discontinues taking drugs during the treatment, some patients come into contact with multidrug-resistant tuberculosis patients in the infectious period, and some patients have mutations in Mycobacterium tuberculosis, drug resistance may occur.
After taking a second-line drug, in the fourth month, Ma Yi began to feel numbness and pain in his feet. Later, due to anemia, he stopped the drug at the doctor’s suggestion. "But the dilemma is that if you stop taking one medicine, you will lose one medicine, because there are only those second-line medicines to choose from."
Drug resistance has become a thorny issue in the prevention and treatment of tuberculosis. Experts say that drug-resistant tuberculosis in China presents a situation of "one high and six low", that is, high incidence rate, low awareness rate, low discovery rate, low inclusion rate, low treatment success rate, low treatment management rate and low independent research and development ability.
In addition, the course of treatment of drug-resistant tuberculosis is as long as 18 to 24 months, and some even reach 36 months. The long course of treatment and the use of second-line drugs, which are much more expensive than first-line drugs, greatly increase the economic burden of patients and reduce their compliance. Many patients stop taking drugs halfway, resulting in more serious consequences.
Where will TB control go?
As one of the countries with high burden of tuberculosis, China has always attached importance to the prevention and treatment of tuberculosis. However, there is still a long way to go to stop TB. There are three magic weapons for the prevention and control of infectious diseases: controlling the source of infection, cutting off the route of transmission and protecting susceptible people. From the technical point of view of prevention and treatment, diagnosis is particularly critical. During the two sessions of the National People’s Congress this year, Dong Xiaoping, member of Chinese People’s Political Consultative Conference and chief virologist of China Center for Disease Control and Prevention, said that the termination of tuberculosis needs to rely on new diagnostic techniques. Zhang Wenhong, member of Chinese People’s Political Consultative Conference, director of the National Center for Infectious Diseases and director of the Department of Infectious Diseases of Huashan Hospital, suggested that the cost of active screening, pathogen detection and drug resistance screening of tuberculosis patients should be increased in the existing public health projects for early detection, early identification and early intervention.
These coincide with Zhao Yanlin, director of the Center for Disease Control and Prevention of China, who put forward the "TB-free community creation action". He pointed out that the community is not only the basic unit of society, but also the main place for home treatment and management of tuberculosis patients, and it is the key link to gradually eliminate the harm of tuberculosis from point to point. At present, grass-roots community medical and health institutions have been included in the service system of tuberculosis prevention and treatment in China, and have been given tasks such as screening suspicious symptoms of tuberculosis, tracking and managing tuberculosis patients, publicizing knowledge of tuberculosis prevention and treatment, and assisting in screening key populations. At present, China has done the pilot work of TB-free communities in 36 sites in 18 provinces, covering more than 1.8 million people.
How to create a TB-free community? Zhao Yanlin proposed that the main measures are "three screens, two tubes and one mobilization", "three screens" refers to actively finding tuberculosis patients, strengthening screening of drug-resistant tuberculosis and detecting tuberculosis infection in high-risk groups, "two tubes" refers to standardizing the treatment and management of tuberculosis and drug-resistant tuberculosis and promoting preventive treatment management, and "one mobilization" refers to the mobilization of the whole society.
"By taking comprehensive measures, starting from the basic units of society, some communities will be TB-free, from point to line, from line to surface, from the establishment of TB-free communities to TB-free districts and counties, and then to TB-free cities, TB-free provinces and TB-free countries, moving towards the China path of ending TB epidemic goals." Zhao Yanlin said.
Quzhou City, Zhejiang Province, carried out the "active screening, free treatment and hospitalization" tuberculosis prevention and control promotion action. Bin Chen, deputy director of the Institute of Tuberculosis Prevention and Control, Zhejiang Provincial Center for Disease Control and Prevention, introduced that in 2020, Quzhou launched a free tuberculosis screening project for rural elderly people over 65 years old, providing 55 yuan funds for each person, so as to actively find tuberculosis patients in the community. In the aspect of free treatment for common tuberculosis patients, three counties in six counties of Quzhou City have begun to implement the policy of zero burden of treatment for common tuberculosis patients. For patients with drug-resistant tuberculosis, it is proposed that patients with drug-resistant tuberculosis should realize zero burden of treatment, and all expenses should be covered by finance. In terms of hospitalization supplement, Bin Chen pointed out that the standard of hospitalization days for general patients is 7-mdash; 10 days, while patients with bacterial positive pulmonary tuberculosis generally need to be hospitalized for isolation treatment for 14-mdash; In 28 days, the patient’s prolonged hospitalization will exceed the medical insurance payment, which leads to the patient’s discharge without turning negative. Therefore, Quzhou City provides special subsidies to designated hospitals. The subsidy standard is calculated according to the average increase of 7 days’ hospitalization time for each inpatient on the existing basis, and 600 yuan is subsidized every day, so that patients can be hospitalized in isolation until they turn negative, which reduces the risk of transmission.
Active screening has moved the gateway forward, changing the focus from "treatment" to "prevention". In the past three years, Quzhou City has screened about 600,000 people over 65 years old, and the number of tuberculosis patients screened basically accounts for 20% of the number of tuberculosis patients found in that year. The zero-burden treatment and hospitalization subsidy policy have eliminated the worries of patients and greatly improved the hospitalization rate of patients.
Active prevention, medical treatment and medical protection. In fact, at present, many areas in China are actively exploring the ways to ensure the diagnosis and treatment of tuberculosis. For example, Xinjiang takes free hospitalization and isolation treatment measures for tuberculosis patients; Ningxia implements the way of medical insurance first, the government covering the bottom, and grading the burden of financing, so as to realize that the out-of-pocket (fee) ratio of the total medical expenses of ordinary pulmonary tuberculosis patients is less than 30%, and the out-of-pocket (fee) of patients with multidrug resistance and difficulties is less than 10%; Jiangsu province has comprehensively promoted the prevention and treatment of drug-resistant tuberculosis, started the free molecular diagnosis test of GeneXpert Mycobacterium tuberculosis, and implemented the free supply of second-line anti-tuberculosis drugs for drug-resistant tuberculosis patients.
Ending tuberculosis has a long way to go, but it is imperative. (Both Wang Xiu and Ma Yi are pseudonyms. )
(Reporter/Intern reporter in Zhang Ke/Graphic Design in Meng-Di Zhang/Proofreading in Yan Ni/Yan Tiantian)